
7, 8 Frequency of episodes is variable, ranging from <1 episode per year to several per day, but most patients have several episodes per week. However, more commonly after the abrupt discontinuation of antidepressant medication (tricyclic antidepressants, serotonin reuptake inhibitors, or serotonin-norepinephrine reuptake inhibitor ), attacks of cataplexy typically are more frequent and/or more intense (rebound phenomena) and can last up to several hours, at which time they are designated as status cataplecticus. 2 Duration of a cataplectic attack generally lasts from a few seconds to several minutes. 2, 5 Patients typically sense the onset of an episode, allowing them to sit or brace themselves before its occurrence, thus reducing the risk of injury, although in one survey, up to half of patients reported some kind of injury from their cataplexy. 2, 5, 6 Positive motor symptoms such as muscle twitching or small jerks of the face or limbs also occur, sometimes contributing to misdiagnosis. 3 The most common manifestations are neck weakness, causing head drop partial or complete ptosis facial weakness with sagging of the jaw with or without dysarthria and trembling or buckling of the knees. While any or all voluntary muscles can be affected (with the exception of the diaphragm and the extraocular muscles of the eye), patients remain conscious and continue to breathe and to move their eyes.


2– 4 Episodes are typically brief, generally lasting <2 minutes, followed by rapid return of normal muscle tone/function, and range from mild or barely noticeable to severe, with complete postural collapse. While laughter is the most typical trigger, other triggers include happiness, elation, fright, anger, startle, stress and, less frequently, pain and orgasm, although episodes may also occur spontaneously. Further research and development of therapeutic approaches to cataplexy are needed.Ĭataplexy: definition and characteristicsĬataplexy is defined as episodes of sudden, transient loss of voluntary muscle tone (usually bilateral, but case reports have identified unilateral cases 1) triggered by strong emotions. Additional possible mechanisms for cataplexy therapy suggested by preliminary research include antagonism of the histamine H 3 autoreceptor with pitolisant and intravenous immunoglobulin therapy for amelioration of the presumed autoimmune-mediated hypocretin/orexin cell loss.

#Cataplexy treatment trial#
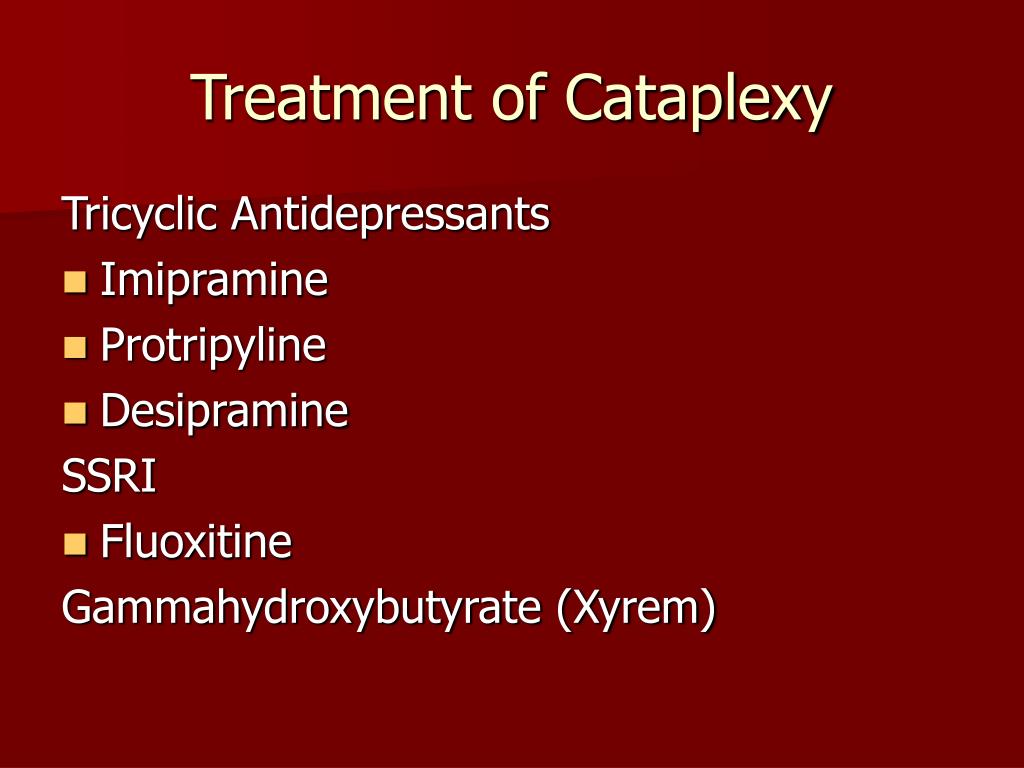
Clinical trial evidence of its efficacy and safety in cataplexy is robust, and it is hypothesized that its therapeutic effects may occur through gamma-aminobutyric acid receptor type B-mediated effects at noradrenergic, dopaminergic, and thalamocortical neurons. The single pharmacotherapy indicated for cataplexy and the guideline-recommended first-line treatment in Europe and the US is sodium oxybate, the sodium salt of gamma-hydroxybutyrate. However, systematic research evidence supporting antidepressants for cataplexy is lacking. Multiple classes of antidepressants have been commonly used off-label for cataplexy in narcolepsy and are suggested for this use in expert consensus guidelines based on traditional practice, case reports, and small trials. Despite these advances, a literature review shows that treatment of cataplexy remains limited. Although the cause of hypocretin/orexin neuron loss in narcolepsy with cataplexy is unknown, an autoimmune etiology is widely hypothesized. It is now generally considered that loss of signaling by hypothalamic hypocretin/orexin-producing neurons plays a key role in the development of cataplexy. Knowledge of the pathophysiology of cataplexy has advanced through study of canine, murine, and human models. Cataplexy is most commonly associated with and considered pathognomonic for narcolepsy, a sleep disorder affecting ~0.05% of the general population.
Cataplexy is defined as episodes of sudden loss of voluntary muscle tone triggered by emotions generally lasting <2 minutes.


 0 kommentar(er)
0 kommentar(er)
